Working Time
| Monday to Friday | 10:00 - 17:00 |
| Saturday | 10:00 - 14:00 |
| Sunday | Closed |
Query Form
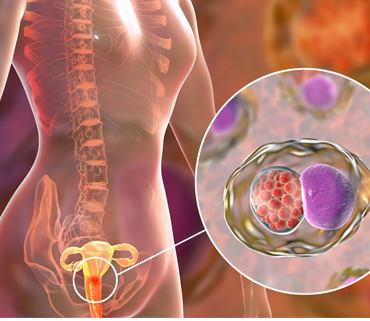
Cervix Cancer
What is cervical cancer or cancer of cervix?
Cervical cancer is a type of cancer that occurs in the cells of the cervix — the lower part of the uterus that connects to the vagina.
Various strains of the human papillomavirus (HPV), a sexually transmitted infection, play a role in causing most cervical cancer.
When exposed to HPV, the body's immune system typically prevents the virus from doing harm. In a small percentage of people, however, the virus survives for years, contributing to the process that causes some cervical cells to become cancer cells.
- You might be at higher risk of cervical cancer if you:
- Started having sex before age 16 or within a year of starting your period
- Have multiple sexual partners
- Take birth control pills, especially for longer than 5 years
- Smoke cigarettes
- Have a weakened immune system
- Have a sexually transmitted disease (STD)
In India, cervical cancer contributes to approximately 6–29% of all cancers in women. The age-adjusted incidence rate of cervical cancer varies widely among registries; highest is 23.07/100,000 in Mizoram state and the lowest is 4.91/100,000 in Dibrugarh district.
You might not notice symptoms of cervical cancer until it’s far along. They may include: Pain when you have sex, Unusual vaginal bleeding, such as after sex, between periods, after menopause, or after a pelvic exam, Unusual vaginal discharge
After it has spread, the cancer can cause:
Pelvic pain, Trouble peeing, Swollen legs, Kidney failure, Bone pain, Weight loss and lack of appetite, Fatigue
If cervical cancer is suspected, your doctor is likely to start with a thorough examination of your cervix. A special magnifying instrument (colposcope) is used to check for abnormal cells.
During the colposcopic examination, your doctor is likely to take a sample of cervical cells (biopsy) for laboratory testing. To obtain tissue, your doctor may use:
- Punch biopsy, which involves using a sharp tool to pinch off small samples of cervical tissue.
- Endocervical curettage, which uses a small, spoon-shaped instrument (curet) or a thin brush to scrape a tissue sample from the cervix.
If the punch biopsy or endocervical curettage is worrisome, your doctor may perform one of the following tests:
- Electrical wire loop, which uses a thin, low-voltage electrified wire to obtain a small tissue sample. Generally this is done under local anesthesia in the office.
- Cone biopsy (conization), which is a procedure that allows your doctor to obtain deeper layers of cervical cells for laboratory testing. A cone biopsy may be done in a hospital under general anesthesia.
Staging
If your doctor determines that you have cervical cancer, you'll have further tests to determine the extent (stage) of your cancer. Your cancer's stage is a key factor in deciding on your treatment.
Staging exams include:
- Imaging tests. Tests such as X-ray, CT scan of Abdomen and Pelvis, MRI Abdomen and Pelvis and positron emission tomography (PET) help your doctor determine whether your cancer has spread beyond your cervix.
- Visual examination of your bladder and rectum. Your doctor may use special scopes to see inside your bladder and rectum.
Treatment for cervical cancer depends on several factors, such as the stage of the cancer, other health problems you may have and your preferences. Surgery, radiation, chemotherapy or a combination of the three may be used.
Surgery
Early-stage cervical cancer can be treated with surgery or Radiotherapy with equal local control rates. Which operation is best for you will depend on the size of your cancer, its stage and whether you would like to consider becoming pregnant in the future.
Options might include:
- Surgery to cut away the cancer only. For a very small cervical cancer, it might be possible to remove the cancer entirely with a cone biopsy. This procedure involves cutting away a cone-shaped piece of cervical tissue, but leaving the rest of the cervix intact. This option may make it possible for you to consider becoming pregnant in the future.
- Surgery to remove the cervix (trachelectomy). Early-stage cervical cancer might be treated with a radical trachelectomy procedure, which removes the cervix and some surrounding tissue. The uterus remains after this procedure, so it may be possible to become pregnant, if you choose.
- Surgery to remove the cervix and uterus (hysterectomy). Most early-stage cervical cancers are treated with a radical hysterectomy operation, which involves removing the cervix, uterus, part of the vagina and nearby lymph nodes. A hysterectomy can cure early-stage cervical cancer and prevent recurrence. But removing the uterus makes it impossible to become pregnant.
Minimally invasive hysterectomy, which involves making several small incisions in the abdomen rather than one large incision, may be an option for early-stage cervical cancer. People who undergo minimally invasive surgery tend to recover more quickly and spend less time in the hospital. But some research has found minimally invasive hysterectomy may be less effective than traditional hysterectomy. If you're considering minimally invasive surgery, discuss the benefits and risks of this approach with your surgeon.
Radiation Therapy
Radiation therapy uses high-powered energy beams, such as X-rays to kill cancer cells. Radiation therapy is often combined with chemotherapy as the primary treatment for locally advanced cervical cancers. It can also be used after surgery if there's an increased risk that the cancer will come back.
Radiation therapy can be given:
- Externally, by directing a radiation beam at the affected area of the body (external beam radiation therapy). Usually around 4-5 weeks of radiation therapy is required.
- Internally, by placing a device filled with radioactive material inside your vagina, usually for only a few minutes (brachytherapy)
- Both externally and internally
If you haven't started menopause yet, radiation therapy might cause menopause. If you might want to consider becoming pregnant after radiation treatment, ask your doctor about ways to preserve your eggs before treatment starts.
Chemotherapy
Chemotherapy is a drug treatment that uses chemicals to kill cancer cells. It can be given through a vein or taken in pill form. Sometimes both methods are used.
For locally advanced cervical cancer, low doses of chemotherapy are often combined with radiation therapy, since chemotherapy may enhance the effects of the radiation (Radiosenstizer). Higher doses of chemotherapy might be recommended to help control symptoms of very advanced cancer.
Targeted therapy
Targeted drug treatments focus on specific weaknesses present within cancer cells. By blocking these weaknesses, targeted drug treatments can cause cancer cells to die. Targeted drug therapy is usually combined with chemotherapy. It might be an option for advanced cervical cancer.
Immunotherapy
Immunotherapy is a drug treatment that helps your immune system to fight cancer. Your body's disease-fighting immune system might not attack cancer because the cancer cells produce proteins that make them undetectable by the immune system cells. Immunotherapy works by interfering with that process. For cervical cancer, immunotherapy might be considered when the cancer is advanced and other treatments aren't working.
The survival rate is close to 100% when you find and treat precancerous or early cancerous changes. The prognosis for invasive cervical cancer depends on the stage.
- More than 90% of women with stage 0 survive at least 5 years after diagnosis.
- Stage I cervical cancer patients have a 5-year survival rate of 80% to 93%.
- Women with stage II cervical cancer have a 5-year survival rate of 58% to 63%.
- The survival rate for women with stage III cervical cancer is 32% to 35%.
- Sixteen percent or fewer women with stage IV cervical cancer survive 5 years.
The key to preventing invasive cervical cancer is to detect cell changes early, before they become cancerous. Regular pelvic exams and Pap tests are the best way to do this. Cervical cancer screening is usually part of a woman's health checkup. There are two types of tests: the Pap test and the HPV test. For both, the doctor or nurse collects cells from the surface of the cervix. With the Pap test, the lab checks the sample for cancer cells or abnormal cells that could become cancer later.
Experts recommend this schedule:
- Get a Pap test every 3 years once you’re 21 or older.
- If you’re 30 to 65, you can get both a Pap test and a human papillomavirus (HPV) test every 5 years. Beyond that age, you may be able to stop testing if your doctor says you’re at low risk.
- Women of any age don’t need screening if they’ve had their cervix removed and have no history of cervical cancer or precancerous lesions.
- If you’re sexually active and have a higher risk for STDs, get tests for chlamydia, gonorrhea, and syphilis each year. Take an HIV test at least once, or more often if you’re at high risk.
Avoiding HPV is also important. Steps to prevent infection include:
- Don’t have sex. If you have sex, use a barrier like a condom
- Get the HPV vaccine. The FDA has approved Gardasil for males and females ages 9 to 26. It protects against two strains of HPV that cause 70% of cervical cancers and over 50% of precancerous lesions of the cervix, vulva, and vagina. Gardasil also protects against the types of HPV that are linked to over 90% of cases of genital warts.
Because cigarette smoking also raises your odds of having cervical cancer, quitting can lower your risk.